
Key Findings
Three in five adults age 50–80 (60%) reported using an alternative site of care (47% urgent care, 28% retail clinic, 9% worksite clinic, and 5% mobile clinic) in the past two years.
Among older adults with a primary care provider (PCP) who visited an alternative site 71% had contact with their PCP about their visit to an alternative site.
Nearly two in three of all adults age 50–80 (62%) and 43% of those who had not used an alternative site for health care in the past two years said they were likely to use an alternative site for health care in the future.
In recent years, “alternative” sites for health care — such as urgent care and retail health clinics — have expanded to meet growing demand for more convenient and accessible care outside of traditional settings like doctors’ offices or hospital emergency departments. Alternative sites of care became particularly popular during the COVID-19 pandemic as locations for rapid testing and treatment, and these settings continue to see high demand. In August 2023, the University of Michigan National Poll on Healthy Aging asked a national sample of adults age 50–80 about their use of and opinions about alternative sites of care.
Use of alternative sites of care
Overall, three in five adults age 50–80 (60%) reported that in the past two years they used an alternative site of care, defined in this poll as an urgent care clinic (not including a hospital emergency department), retail health clinic (typically found in retail locations such as pharmacies, grocery stores, or department stores), worksite clinic, or mobile clinic (in a bus or van). Nearly half of all older adults (47%) reported visiting an urgent care clinic in the past two years, with 23% having gone to urgent care more than once during this period. Over one in four older adults (28%) visited a retail health clinic in the past two years, while fewer had visited a worksite clinic (9%) or a mobile clinic (5%).

Those more likely to have used any alternative site for health care included people age 50–64 (64% vs. 55% of those age 65–80), women (63% vs. 57% of men), and those with higher annual household incomes (65% of those with an annual income of $60,000 or more vs. 53% with incomes less than $60,000). Older adults living in urban or suburban areas (population over 50,000) were also more likely to have visited an alternative site of care (62% vs. 52% in less populated areas).
When asked about their most recent alternative site visit, 34% sought follow-up care afterwards: 21% received follow-up care from their usual health care provider, 7% received care from the same alternative site, and 6% went somewhere else. More than half (58%) said they did not need follow-up care, and 9% chose not to get follow-up care.
Among those who visited an alternative site of care in the past two years, 91% reported having a primary care provider (PCP). Of those with a PCP, 71% had contact with their PCP about their visit to an alternative site for health care. More than one in five (22%) had a follow-up visit with their usual health provider. Among those who did not have a follow-up visit, 43% let their PCP know they had visited an alternative site of care and 29% had their visit records sent to their PCP.
Reasons for using an alternative site for health care
Among those who had visited an alternative site of care in the past two years, the most common reasons were to avoid the hospital emergency department (44%) or to get a vaccine, specific test, or health exam (35%). Other reasons included the ability to get an appointment sooner or at a more convenient time (31%), their regular provider’s office was closed (26%), the alternative site was closer (15%), and their regular provider instructed them to go (10%). Fewer cited cost (9%), travel/being out of town (6%), that they usually go to an alternative site
for health care (4%), or that they went to receive care aligned with their culture or language (1%).
When asked about the type of care or treatment sought at an alternative site, 41% said it was for symptoms of an illness, 38% went to get a vaccine, 21% for an injury, 14% for COVID-19 infection/possible infection, 11% for a specific screening, test, or exam (other than for COVID-19), 8% for prescription renewals, 3% for physical exams for work or travel, and 2% for mental health concerns.
Alternative sites versus PCPs
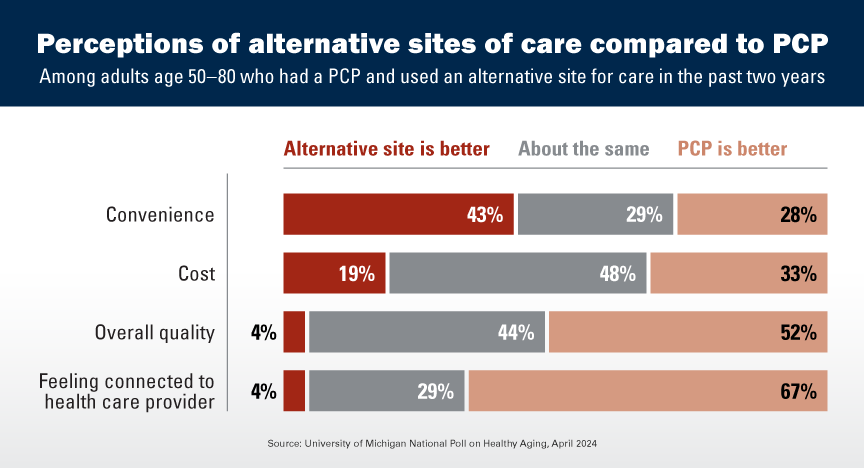
Three in five older adults who reported having a PCP (61%) visited an alternative site of care in the last two years. This group was asked to compare those settings on several factors. For overall convenience, 43% noted an alternative site of care was better, 28% thought the PCP was better, and 29% said they were about the same. On cost, 19% said an alternative site was better, 33% indicated their PCP was better, and 48% said the costs were about the same. For overall quality, 4% said an alternative site was better, 52% preferred their PCP, and 44% said both were about the same. On feeling connected to the health care provider, 4% noted an alternative site was better, 67% preferred their PCP, and 29% said they were about the same.
Future use of alternative sites of care
Nearly two in three adults age 50–80 (62%) said they were at least somewhat likely (11% very likely, 51% somewhat likely) to use an alternative site for health care in the future. Those who had visited an alternative site for health care in the past two years were more likely to indicate they would be very or somewhat likely to use one in the future compared with those who had not visited one during this time period (75% vs. 43%). People age 50–64, women, those in excellent, very good, or good physical health, and those with higher levels of education and with higher household incomes were also more likely to report that they would use an alternative site for health care in the future.
Among the 38% of older adults who said that they were not likely to use an alternative site for health care in the future, 74% said they preferred getting care from their usual health care provider. Other reasons included not being familiar with alternative sites (30%), their insurance does not cover them or they are worried about cost (23%), they do not trust alternative sites (18%), or they have concerns about the privacy of their health data (10%). About one in ten (9%) said that an alternative site of care is hard to get to or that there is not one close by.
Implications
Use of alternative sites of care is common among adults age 50–80. Three in five older adults received health care at an alternative site in the past two years; almost half reported use of an urgent care clinic during this period. Among those who had used an alternative site of care, three out of four said they would be likely to visit one again in the future—while one in four said they would not be likely to do so.
Among older adults who used an alternative site of care in the past two years, the most common reasons were related to the timeliness of care. Most felt that these sites offered greater or equal overall convenience compared to their PCP. However, most also felt that their regular PCP’s office was better when it came to care quality, cost, and feeling connected to the health care provider. While the majority of older adults with a PCP reported some communication with their PCP about their visit to an alternative site of care, more than one in four did not.
Alternative sites of care were important sources of timely, convenient care during the COVID-19 pandemic, and the experiences and perceptions of older adults suggest these sites will continue to play a significant role in the future. Therefore, it is vital for clinicians, researchers, and policymakers to monitor older adults’ experiences with quality and cost of care at alternative sites of care, as well as take meaningful steps to ensure that care received at these sites is well-coordinated with care received from one’s usual health care provider.
Data Source and Methods
This National Poll on Healthy Aging report presents findings from a nationally representative household survey conducted exclusively by NORC at the University of Chicago for the University of Michigan’s Institute for Healthcare Policy and Innovation. National Poll on Healthy Aging surveys are conducted using NORC’s AmeriSpeak probability-based panel. This survey module was administered online and via phone from July 17th–August 7th, 2023 to a randomly selected, stratified group of U.S. adults age 50–80 (n=2,657), with an oversample of non-Hispanic Black and Hispanic populations. The sample was subsequently weighted to reflect population figures from the U.S. Census Bureau. The completion rate was 50% among panel members contacted to participate. The margin of error is ±1 to 5 percentage points for questions asked of the full sample and higher among subgroups.
Findings from the National Poll on Healthy Aging do not represent the opinions of the University of Michigan or AARP. The University of Michigan reserves all rights over this material.
Read other National Poll on Healthy Aging reports and about our Michigan findings, and learn about the poll methodology.
Citation
Dean O, Komisar H, Singer D, Solway E, Box N, Roberts S, Hutchens L, Smith E, Kirch M, Kullgren J. Alternative Sites for Health Care. University of Michigan National Poll on Healthy Aging. April 2024. Available at https://dx.doi.org/10.7302/22501.