
An estimated one in five older adults currently experience depression, anxiety, insomnia, substance use, or another mental health disorder. These conditions are not a normal part of aging and can impair physical and social functioning. Identifying and treating them can improve quality of life and overall well-being. The COVID-19 pandemic has created unprecedented challenges for older adults that can negatively affect mental health. In January 2021, the University of Michigan National Poll on Healthy Aging asked a national sample of U.S. adults age 50–80 about their mental health and the effect of the COVID-19 pandemic on their mental health symptoms.
Perceptions of mental health
Two in three adults age 50–80 (65%) rated their mental health as excellent or very good, 27% as good, and 8% as fair or poor. Few older adults (5%) said their overall mental health was better compared to before the pandemic, and 18% said it was worse. Reporting worse mental health since the pandemic began was more common among women, those age 50–64, those with higher education, and those who rated their physical health as fair or poor. (Table).
About one in five older adults (19%) rated their overall mental health as better compared to 20 years ago, 62% rated it the same, and 19% said it was worse. Rating mental health as worse now than 20 years ago was more common among those who rated their physical health as fair or poor and those with an annual household income less than $30,000.
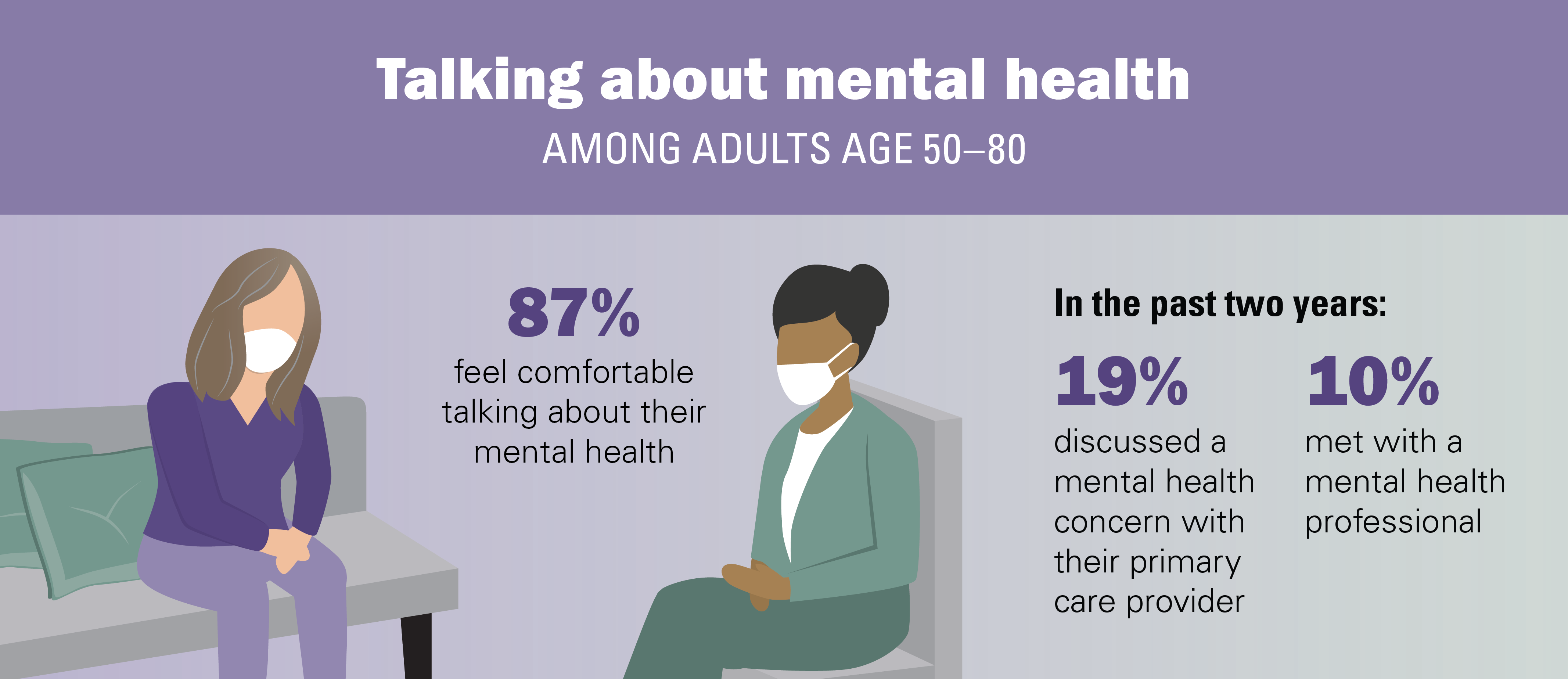
Comfort discussing mental health
Most older adults (87%) reported feeling comfortable (53% very comfortable, 34% somewhat comfortable) talking about their mental health. When asked with whom they would most want to talk about mental health concerns, adults age 50–80 preferred to talk with their primary care provider (31%), a mental health professional (25%), spouse or partner (25%), or other family or friends (11%). Within the past two years, nearly one in five older adults (19%) said they discussed a mental health concern with their primary care provider, while 10% had seen a mental health professional. Among all respondents, the majority (71%) indicated they would not have hesitations about seeing a mental health professional for treatment in the future, and 29% said they were unsure (24%) or had some reservations (5%). Among those who were unsure or had reservations about seeing a mental health professional, the most common reasons were thinking it would not help (21%), feeling embarrassed (16%), and cost (14%).
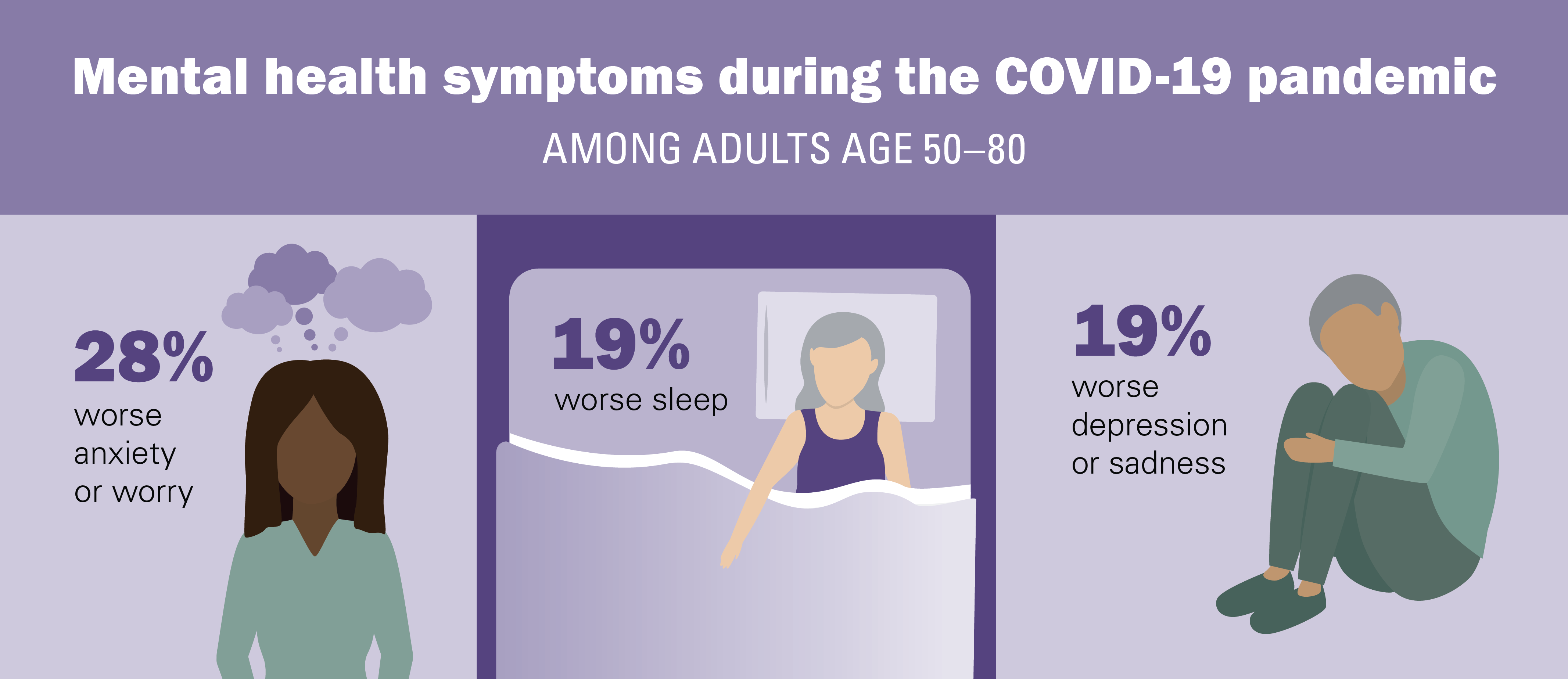
Impact of the pandemic on mental health symptoms
Older adults commonly reported depression, anxiety, and trouble with sleep during the COVID-19 pandemic. Since March 2020, nearly one in five adults age 50–80 (19%) reported worse sleep than compared to before the COVID-19 pandemic. Two in three (64%) said they regularly had trouble falling or staying asleep one or more nights in the past week. Additionally, one in five (19%) reported experiencing worse depression or sadness, and 28% reported worse anxiety or worry, since the start of the pandemic. Worse sleep, depression, and anxiety during the pandemic were also more common among women than men, those age 50–64 compared to age 65–80, and those who rated their physical health as fair or poor compared to those in excellent, very good, or good health.
More than one in four older adults said that for several days or more within the past two weeks they had little pleasure in doing things (29%) or felt depressed or hopeless (28%). One in three (34%) reported feeling nervous, anxious, or on edge, and 44% said they felt stressed. More than one in three older adults (37%) reported feeling a lack of companionship and 46% reported feeling isolated from others in the past year.
Strategies to improve mental health
Older adults reported engaging in a variety of strategies to improve their mental health from March 2020 to January 2021. During this period, one in eight (13%) discussed a new mental health concern with their primary care provider, 6% adjusted or started a new prescription medication for their mental health, and 5% started seeing a mental health professional. Three in ten older adults (29%) reported making a lifestyle change to improve their well-being such as exercise, diet, or meditation. Making lifestyle changes during the pandemic was more common among adults 50–64 than those age 65–80 (31% vs. 25%), women compared to men (33% vs. 24%), and Blacks and Hispanics compared to Whites (38% vs. 34% vs. 27%).
Implications
In this poll, the majority of U.S. adults age 50–80 reported that their mental health was excellent or very good, and their overall mental health was as good, if not better, than it was 20 years ago. Resiliency, wisdom, and life experience may help contribute to improved mental health with age. However, physical and mental health were closely related—those with poor physical health also rated their mental health as worse both now and compared to two decades earlier.
The COVID-19 pandemic has had a negative impact on the well-being of many older adults. About one in five poll respondents said their overall mental health was worse since the pandemic started, consistent with the one in five who reported experiencing worse sleep, depression, and anxiety since March 2020. Nearly half of adults age 50–80 reported feeling regularly stressed and isolated from others. These symptoms were common and experienced more frequently by women, those with lower annual household incomes, and those with worse physical health. Contributors to worse mental health during this time may have included pandemic-related challenges (isolation, concerns about illness) as well as stress from economic and political conditions.
While mental health conditions are treatable, nearly one in three older adults said they might have some hesitation about seeking mental health care in the future. This suggests there is still more to be done to address stigma and ensure access to affordable mental health care. Most older adults said they were comfortable discussing their mental health. To address stigma and help people to get the care they need, health care providers should routinely screen for mental health symptoms and connect older adults with effective treatment options. More health systems across the U.S. are merging mental health care into primary care, which can help greater numbers of older adults accept and access mental health treatment.
There are strategies that older adults can use to manage stress and support their mental health, even in the midst of major personal and societal challenges. Establishing routines, maintaining a regular sleep schedule, and setting goals can provide beneficial daily structure. Regular exercise, adequate sleep, natural light, and minimizing alcohol use can all help to improve mental health and well-being. Deep breathing, meditation, and muscle relaxation can help to manage stress and anxiety. Older adults with more persistent mental health symptoms should discuss additional treatment options with their health care providers, including medications and psychosocial interventions like cognitive behavioral therapy.
Given the isolation experienced by many older adults during the pandemic, staying connected with friends and family by regularly reaching out to others and asking for help when needed can maintain social connections. For those worried that a loved one or friend could be experiencing depression or other mental health symptoms, it can be helpful to regularly check in and encourage them to discuss mental health concerns with their health care providers.
With the rise in mental health symptoms experienced by older adults during the pandemic, ensuring access to mental health services, including through telehealth, is essential both now and in the future.
Data Source and Methods
This National Poll on Healthy Aging report presents findings from a nationally representative household survey conducted exclusively by Ipsos Public Affairs, LLC (“Ipsos”) for the University of Michigan’s Institute for Healthcare Policy and Innovation. National Poll on Healthy Aging surveys are conducted by recruiting from Ipsos KnowledgePanel®, the largest national, probability-based panel in the U.S.
This survey module was administered online in January 2021 to a randomly selected, stratified group of older adults age 50–80 (n=2,023). The sample was subsequently weighted to reflect population figures from the U.S. Census Bureau.
The completion rate was 78% among panel members contacted to participate. The margin of error is ±1 to 3 percentage points for questions asked of the full sample and higher among subgroups.
Findings from the National Poll on Healthy Aging do not represent the opinions of the University of Michigan. The University of Michigan reserves all rights over this material.
Read other National Poll on Healthy Aging reports and about the poll's Michigan findings, and learn about the poll methodology.
Citation
Gerlach L, Solway E, Singer D, Kullgren J, Kirch M, Malani P. Mental Health Among Older Adults Before and During the COVID-19 Pandemic. University of Michigan National Poll on Healthy Aging. May 2021. Available at: http://dx.doi.org/10.7302/983
Scholarly Publications
Gerlach LB, Solway E, Maust DT, et al. The COVID-19 pandemic and mental health symptoms among US adults. J Gen Intern Med. 2021;36:3285–3288. doi:10.1007/s11606-021-07046-3
Gerlach LB, Maust DT, Solway E, et al. Perceptions of overall mental health and barriers to mental health treatment among US older adults. Am J Geriatr Psychiatry. Apr 2022;30(4):521-526. doi:10.1016/j.jagp.2021.09.006.