
Advance care planning helps ensure people receive medical care that is consistent with their values, goals, and preferences. Such planning includes important discussions of treatment preferences with family, friends, or health care providers. It also often includes legal documentation of a medical durable power of attorney (designation of a trusted person to make medical care decisions on behalf of the individual when they cannot) and an advance directive (a written statement of an individual’s wishes regarding medical treatment, also called a living will). In June 2020, the National Poll on Healthy Aging asked a national sample of U.S. adults age 50–80 about their advance care planning before and during the early months of the COVID-19 pandemic.
Talking about care preferences
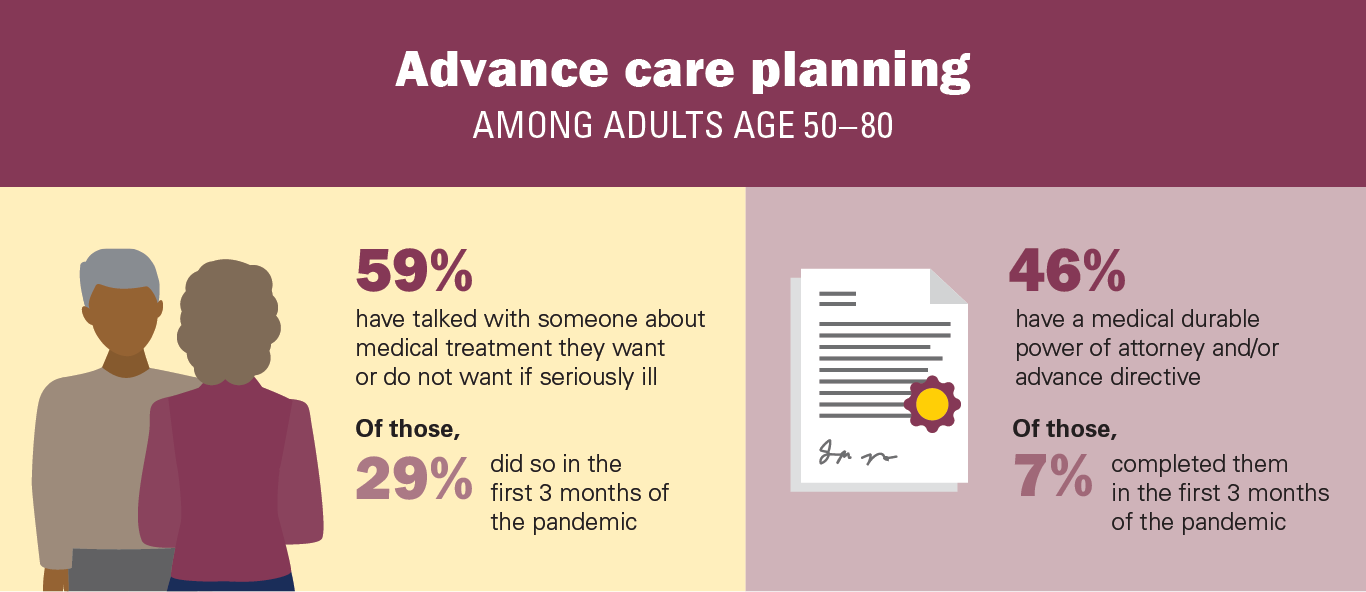
Nearly three in five adults age 50–80 (59%) said they have talked to someone (i.e., a spouse, adult children, other family, or friends) about the types of medical care they want or do not want if they become seriously ill. People age 65–80 were more likely than those age 50–64 (70% vs. 51%) and women were more likely than men (62% vs. 55%) to have talked to someone about their care preferences.
Among older adults who had talked with someone about their health care preferences, 40% most recently discussed it a year or more ago, 31% within the past 3–11 months, and 29% within the past three months (March–May 2020). Of those who had a conversation in the past three months, 41% said it was because of COVID-19. Among older adults who had not had a conversation about their care preferences, 56% reported it was because they had not gotten around to it, 23% said they do not like talking about these things, and 21% did not think it was necessary.
Legal documents
Nearly half of older adults (46%) reported they had completed at least one advance care planning legal document (i.e., a medical durable power of attorney or advance directive), with 37% completing both and 9% completing one of these documents. Among those who had completed at least one of these documents, 80% completed or updated more than a year ago, 13% within the past 3–11 months, and 7% in the past 3 months (March–May 2020).
Reasons for completing or updating medical durable power of attorney and/or advance directive documents included feeling it was important to do (70%); hospitalization, surgery, or a health concern for themselves (15%); loss of a loved one (10%); suggestion from a health care provider (8%); hospitalization of a family member or friend (6%); and changes in their care preferences (4%). Among individuals who completed or updated their medical durable power of attorney and/or advance directive documents within the past three months, 35% said it was due to concerns about COVID-19.
Among the 54% of older adults who had not completed medical durable power of attorney or advance directive documents, 62% said they had not gotten around to it, 15% did not know how, 13% said they do not like talking about these things, 13% did not think it necessary, 9% said no one asked them to, and 7% were deterred by cost.
Implications
This poll showed that nearly two in five adults age 50–80 have not had conversations about their health care preferences if they were to experience a serious illness, and more than two in three have not completed both durable power of attorney and advance directive documents. Among individuals who had not talked about their care preferences with others or completed corresponding legal documents, more than half said it was because they simply had not gotten around to doing these things.
For some individuals, the COVID-19 pandemic could provide an opportunity to make plans to ensure that in the event of a serious medical condition, care is consistent with one’s preferences. We found that during the first three months of the pandemic, one in eight adults age 50–80 talked with someone else about their care preferences. Few older adults reported having created or updated legal documents specifically due to concerns about COVID-19.
New strategies are needed to facilitate conversations about and documentation of preferences for medical care in the event of serious illness, and regular review of previous advance care plans to confirm they remain accurate. Family members, health care providers, legal advocates, and policymakers should encourage these vital discussions and the completion of advance care planning documents to ensure older adults’ care reflects their preferences now and in the future.
Data Source and Methods
This National Poll on Healthy Aging report presents findings from a nationally representative household survey conducted exclusively by Ipsos Public Affairs, LLC (“Ipsos”) for the University of Michigan’s Institute for Healthcare Policy and Innovation. National Poll on Healthy Aging surveys are conducted by recruiting from Ipsos KnowledgePanel®, the largest national, probability-based panel in the U.S.
This survey module was administered online in June 2020 to a randomly selected, stratified group of older adults age 50–80 (n=2,074). The sample was subsequently weighted to reflect population figures from the U.S. Census Bureau.
The completion rate was 78% among panel members contacted to participate. The margin of error is ±1 to 2 percentage points for questions asked of the full sample and higher among subgroups.
Findings from the National Poll on Healthy Aging do not represent the opinions of the University of Michigan. The University of Michigan reserves all rights over this material.
Read other National Poll on Healthy Aging reports and about the poll's Michigan findings, and learn about the poll methodology.
Citation
Perumalswami C, Burke J, Singer D, Malani P, Kirch M, Solway E, Kullgren J, Skolarus L. Older Adults’ Experiences with Advance Care Planning. University of Michigan National Poll on Healthy Aging. April 2021. Available at: http://hdl.handle.net/2027.42/167012